Lower Urinary Tract Symptoms, Sexual Function, and the Quality of Life of Married Women with Urinary Incontinence
https://gexinonline.com/archive/journal-of-comprehensive-nursing-research-and-care/JCNRC-134
2College of Nursing, Research Institute of Nursing Science, Chonbuk National University, 567 Baekje-daero, deokjin-gu, Jeonju-si, Jeollabuk -do 54896 South Korea.
Keywords: Lower Urinary Track Symptom, Sexual dysfunction, Quality of Life, Women
Abbreviations:
LUTS- Lower Urinary Tract Symptoms QoL - Quality of Life UI - Urinary Incontinence BFLUTS-SF - Scored Form of the Bristol Female Lower Urinary Tract Symptoms Questionnaire FSFI - Female Sexual Function Index
The UI have high prevalence and are recognized as important symptoms to represent lower urinary tract symptoms (LUTS). However, in Korea, the focus is mainly on UI, and studies on LUTS, which are likely to occur in duplicate, are rare. LUTS include various urinary symptoms such as urinary frequency, polyuria, nocturia, UI, etc. [4]. These symptoms lead to physical problems such as skin infection, odor, and pressure ulcer [5], and psychological problems such as anxiety about urine odor and incontinence, behavioral limitations (water intake, coughing, or sneezing), frustration or helplessness, and depression; furthermore, these can reduce the quality of life (QoL) of women with UI [6].
Previous studies have shown that women with stress UI have a lower incidence of sexual intercourse and sexual satisfaction than women without it, and tend to avoid sexual activity [7]. The occurrence of LUTS is a major problem women who increasingly engage in social and economic activities but restrict outdoor activities and hobbies as they worry/are anxious about pad use and smell due to incontinence [8]. In particular, studies on UI in Korea have been conducted on elderly women [9] and postmenopausal women [10,11], but studies on incontinence and related variables of married women, including various age groups (such as 30s and 40s) and physiological changes during pregnancy and childbirth, are rare. In addition, it is important to understand LUTS, sexual function, and QoL, which have been predicted to be related to each other in previous studies on women with UI, in order to increase awareness about UI treatment and to identify related variables that cause sexual dysfunction and low quality of life.
This study aimed to provide basic data for the management of LUTS, sexual dysfunction, and QoL degradation in women with UI. Specifically, this study had the following objectives:
1) to determine the degree of LUTS, sexual function, and the QoL of women with UI, 2) to determine score differences between LUTS, sexual function, and the QoL of women with UI according to their general and UI-related characteristics, and 3) to determine the relationship between LUTS, sexual dysfunction, and the QoL of women with UI.
Data were collected from October to November 2016 after obtaining approval from the Institutional Review Boards (IRB) of the Chonbuk National University (IRB No. 2016-08-011-01), located in Jeonbuk Province of South Korea [7]. The participants were informed of the purpose and procedure of this study, voluntary participation, guaranteed anonymity, and the choice to abandon the trial, and written consent was obtained. It took participants an average of 15– 20 minutes to complete the study questionnaire consisting of items about participants’ general and UI-related characteristics and LUTD, FSFI, and SF-36. Since the information regarding sexual function is sensitive, the questionnaire was filled and sealed in an envelope.
The number of participants needed was calculated according to Cohen’s sampling formula using the sample size calculation program G*power 3.1.3. Based on the calculation results, with a correlation analysis significance level of 0.05, a medium effect size (d) of 0.30, and a power of 0.95, the minimum sample size required for this study was 64.
Mean Differences in LUTS, sexual function, and Physical and Mental QoL according to the General Characteristics
Among the LUTS scores according to the general characteristics, significant mean differences exited with respect to education level, menopause, postmenopausal period and types of UI. And among the sexual function scores according to the general characteristics, significant mean differences exited with respect to age, education level, duration of marriage, menopause, postmenopausal period, Kegel's exercise, sexual intercourse per months and Types of UI (Table 1).
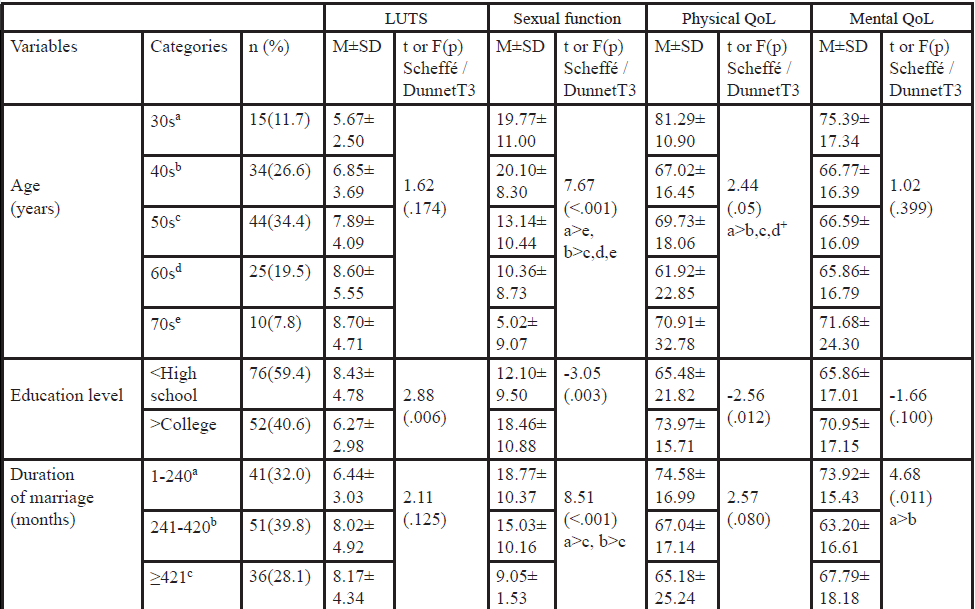 Table 1: Mean Differences in Physical and Mental QoL according to the General Characteristics (N=128).
Table 1: Mean Differences in Physical and Mental QoL according to the General Characteristics (N=128).
+ Dunnet T3 test; LUTS=lower urinary tract symptoms, QoL=Quality of life, UI=Urinary incontinence
Among the physical QoL scores according to the general
characteristics, significant mean differences exited with respect to
age, education level, number of vaginal delivery, menopause, Kegel's
exercise, and types of UI. And among the mental QoL scores according to
the general characteristics, significant mean differences exited
with respect to duration of marriage, menopause, Kegel's exercise,
sexual intercourse per months and Types of UI (Table 1).
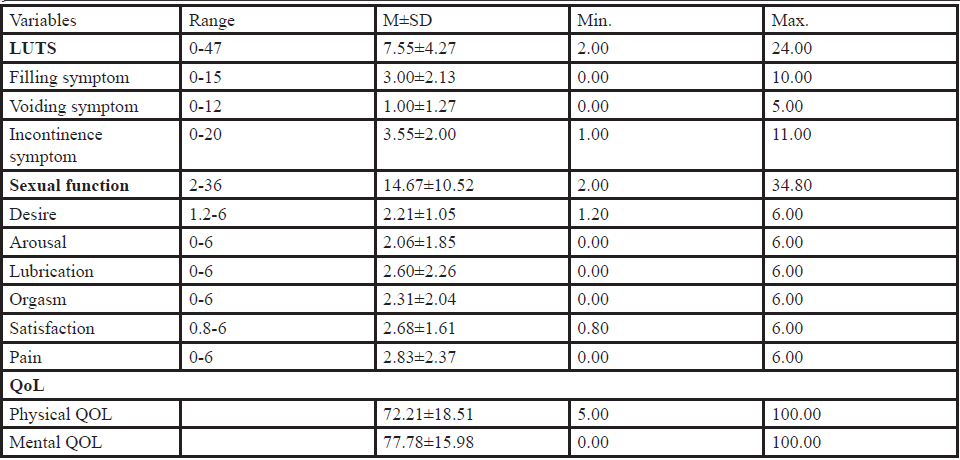 Table 2: LUTS, Sexual Function, and QoL Scores (N=128).
Table 2: LUTS, Sexual Function, and QoL Scores (N=128).
LUTS=lower urinary tract symptoms, QoL=Quality of life, M=Mean, SD=Standard deviation
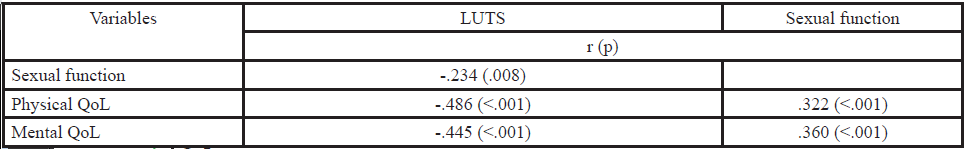 Table 3: Correlation among LUTS, Sexual Function and QoL (N=128).
Table 3: Correlation among LUTS, Sexual Function and QoL (N=128).
LUTS=lower urinary tract symptoms, QoL=Quality of life
In this study, the prevalence according to the type of incontinence in married women was 54.7% for stress UI, 13.3% for urge UI, and 32.0% for mixed UI. The prevalence of UI in previous studies varied according to subject selection and data collection methods. The incidence of UI in this study was similar to that of a previous study [17]. The incidence of urinary incontinence was 55.7%, the incidence of stress UI was 60.8%, the urge and mixed UI were reported to be 1.0% and 38.2%, respectively [17]. However, according to the results of a population-based sampling study of adult women of the same age range (range 30 to 79 years) as in the present study, the incidence of UI was 41.2%, including stress UI (37.8%) and urge UI (14.9%) [12], and the prevalence of UI was lower in this study. The reason for the difference in the prevalence of urinary incontinence in this study is the age associated with incontinence incidence. In the Oh et al. [12] study, mean age was 51.1±12.8 years, while the mean age of women in this study was 53.34±11.11 years. For this reason, the prevalence of incontinence seems to be low. There was a difference in prevalence according to the type of UI, but it is consistent with the fact that stress UI is relatively higher than other types. However, the prevalence of UI in this study and previous studies is different because different tools have been used to determine UI. Thus, in future studies, it may be necessary to identify variables related to UI using objective indicators.
In this study, we discuss the level of LUTS, sexual function, and the QoL of married women who have UI. First, the LUTS score for women with urinary incontinence was 7.55±4.27 points out of 47 points. The results of this study showed that BFLUTS-SF, which uses the same tool as this study, showed LUTS score to be more than the result of 8.38±2.81 points, which is the LUTS score after menopausal transition [18]. Lower estradiol levels during menopausal transition lead to LUTS.
In previous studies, the ratio of menopausal and postmenopausal women was 95% and the rate of fertility was 3.2±2.1, which was related to the development of LUTS.
In this study, sexual function scores of married women with UI were 14.67±10.52 points out of 36 points. In a study of urologic patients using the same tool, 20.48±6.20 points [19], and a sexual function score of 22.39±2.09 points in patients with UI in Korea [20]. The sexual function scores in this study were significantly lower than those in previous studies [19,20]. As a result of comparing the general characteristics of the study subjects with the previous studies and sexual function scores, it was found that the average age of the sexual function, the number of menopausal women, and 47 cases (37.6%), respectively. Because of these differences in general characteristics, sexual function scores in this study seem to be significantly lower. In addition, the sexual function score of this study was 14.67 ± 10.52, which was significantly lower than the cutoff score of sexual dysfunction (26.6 points) [21] suggesting that there are many women with sexual dysfunction. In this study, many of the subjects with UI might be thought to have sexual dysfunction.
In the present study, the QoL scores for women with UI were 68.27±1.60 points out of 100 points. The results of this study were similar to those of previous studies in that the QoL of the women with UI was measured by SF-36, the tool that is also used in the present study, with a score of 69.0±10.6 [22].
In this study, the LUTS, sexual function, and QoL according to the demographic and UI - related characteristics of married women with UI was related to various sociodemographic and UI - related factors. In conclusion, this study should develop a nursing intervention program that can improve the three variables considering the demographic and UI-related characteristics reported to be associated with LUTS, sexual function, and QoL in married women with UI.
The results of this study showed that LUTS was correlated negatively with sexual function and QoL, and sexual function was positively correlated with QoL. That is, the more severe symptoms of lower urinary tract, the lower the sexual function and the QoL, and the better the sexual function, the higher the QoL. The results of this study suggest that there is a negative correlation between LUTS and the QoL of older women in the local community [23], and there is a positive correlation between the sexual function and the QoL of Turkish women with UI [24].
These results suggest that when sexual function and QoL in women with UI is severe are decreased. The LUTS, sexual function and quality of life of women with UI were found to be related to each other. Based on the results of this study, it is expected that nursing education and intervention programs should be introduced in nursing practice of the community to improve the identification of UI, sexual function, and the QoL of married women.
Journal of Comprehensive Nursing Research and Care Volume 3 (2018), Article ID: JCNRC-134
https://doi.org/10.33790/jcnrc1100134Research Article
Lower Urinary Tract Symptoms, Sexual Function, and the Quality of Life of Married Women with Urinary Incontinence
Seon Hwa Kim1, Hye Young Kim2*
1College of Nursing, Chonbuk National University Hospital, 20 Geonji-ro, deokjin-gu, Jeonju-si, Jeollabuk-do 54907 South Korea.2College of Nursing, Research Institute of Nursing Science, Chonbuk National University, 567 Baekje-daero, deokjin-gu, Jeonju-si, Jeollabuk -do 54896 South Korea.
Corresponding Author Details:
Hye Young Kim, College of Nursing, Research Institute of
Nursing Science Chonbuk National University, 567 Baekje-daero
deokjin-gu, Jeonju-si, Jeollabuk-do 54896, South Korea.
E-mail: tcellkim@jbnu.ac.kr
Received date: 25th November, 2018
Accepted date: 31st January, 2019
Published date: 04th February, 2019
Accepted date: 31st January, 2019
Published date: 04th February, 2019
Citation: Kim SH, Kim HY (2019) Lower Urinary Tract Symptoms, Sexual Function, and the Quality of Life of Married
Women with Urinary Incontinence. J Comp Nurs Res Care 4: 134.
Copyright: ©2019, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author
and source are credited
Abstract
The purpose of the study was to identify the level of lower urinary tract symptoms (LUTS), sexual function, and quality of life (QoL) and its correlates in married women with urinary incontinence (UI). Data were collected through self-reported questionnaires that included items on general and UI-related characteristics, and tools to measure LUTS (Scored Form of the Bristol Female Lower Urinary Tract Symptoms Questionnaire, BFLUTS-SF), Sexual function (Female Sexual Function Index, FSFI), and QOL (The Medical Outcomes Study 36-Item Short Form Version 2 Standard, SF-36v2). Data were analyzed using descriptive statistics, t-test, one-way ANOVA, and Pearson correlation coefficients. About 55% of the participants were identified as women with UI. Stress UI was 54.7% and the proportions of urge UI and mixed UI were 13.3% and 32.0%, respectively. The average score for LUTS, sexual function, physical QoL, and mental QoL in married women with UI were found to be 7.55±4.27 points, 14.67±10.52 points, 72.21±18.51 points, and 77.78±15.98 points, respectively. LUTS has a statistically significant negative correlation with sexual function, physical QOL, and mental QoL, respectively, r=-.234, r=-.486, and r=-.445. Sexual function has a statistically significant positive correlation with physical and mental QoL, respectively, r=.322 and r=.360. The results of this study are expected to provide basic data for therapeutic nursing intervention in LUTS management, sexual dysfunction, and low QoL in women with UI, and help to identify and understand the disease of UI.Keywords: Lower Urinary Track Symptom, Sexual dysfunction, Quality of Life, Women
Abbreviations:
LUTS- Lower Urinary Tract Symptoms QoL - Quality of Life UI - Urinary Incontinence BFLUTS-SF - Scored Form of the Bristol Female Lower Urinary Tract Symptoms Questionnaire FSFI - Female Sexual Function Index
Introduction
According to the International Continence Society (ICS), urinary incontinence (UI) is a disease that signifies “involuntary leakage of urine” and is generally classified into stress UI, urge UI, and mixed UI [1]. The length of urethra in women is 3–5 cm, which is five times shorter than that of men. In particular, married women have a higher prevalence of UI compared to men due to physical and physiological changes during pregnancy and childbirth [2]. However, married women have a low awareness of illness and treatment of UI, and consider UI as a natural symptom of normal aging process or childbirth experience, and they miss out on proper treatment due to embarrassment and shame. Therefore, studies on UI should be preceded by research in the community rather than in hospitals [3].The UI have high prevalence and are recognized as important symptoms to represent lower urinary tract symptoms (LUTS). However, in Korea, the focus is mainly on UI, and studies on LUTS, which are likely to occur in duplicate, are rare. LUTS include various urinary symptoms such as urinary frequency, polyuria, nocturia, UI, etc. [4]. These symptoms lead to physical problems such as skin infection, odor, and pressure ulcer [5], and psychological problems such as anxiety about urine odor and incontinence, behavioral limitations (water intake, coughing, or sneezing), frustration or helplessness, and depression; furthermore, these can reduce the quality of life (QoL) of women with UI [6].
Previous studies have shown that women with stress UI have a lower incidence of sexual intercourse and sexual satisfaction than women without it, and tend to avoid sexual activity [7]. The occurrence of LUTS is a major problem women who increasingly engage in social and economic activities but restrict outdoor activities and hobbies as they worry/are anxious about pad use and smell due to incontinence [8]. In particular, studies on UI in Korea have been conducted on elderly women [9] and postmenopausal women [10,11], but studies on incontinence and related variables of married women, including various age groups (such as 30s and 40s) and physiological changes during pregnancy and childbirth, are rare. In addition, it is important to understand LUTS, sexual function, and QoL, which have been predicted to be related to each other in previous studies on women with UI, in order to increase awareness about UI treatment and to identify related variables that cause sexual dysfunction and low quality of life.
This study aimed to provide basic data for the management of LUTS, sexual dysfunction, and QoL degradation in women with UI. Specifically, this study had the following objectives:
1) to determine the degree of LUTS, sexual function, and the QoL of women with UI, 2) to determine score differences between LUTS, sexual function, and the QoL of women with UI according to their general and UI-related characteristics, and 3) to determine the relationship between LUTS, sexual dysfunction, and the QoL of women with UI.
Methods
Study Design
This study involved a descriptive survey that aimed to identify the level of LUTS, sexual function, and QoL and its correlates in married women with UI.Participants and Data Collection
The subjects of this study were married women aged 30 to 79 living in J city, married women living with their spouses, and agreed to participate and understand the purpose of this study. According to the statistics of the National Statistical Office, the proportion of married women in J in June, 2016 (21.7% in 30s, 27.9% in 40s, 24.7% in 50s, 15.7% in 60s, 9.8% in 70s). The incidence of urinary incontinence was defined as the number of patients who answered 'Yes' to the question ‘Do you have involuntary leakage of urine?' [1,4,7]. As a result, there were 128 out of 234 women who had UI.Data were collected from October to November 2016 after obtaining approval from the Institutional Review Boards (IRB) of the Chonbuk National University (IRB No. 2016-08-011-01), located in Jeonbuk Province of South Korea [7]. The participants were informed of the purpose and procedure of this study, voluntary participation, guaranteed anonymity, and the choice to abandon the trial, and written consent was obtained. It took participants an average of 15– 20 minutes to complete the study questionnaire consisting of items about participants’ general and UI-related characteristics and LUTD, FSFI, and SF-36. Since the information regarding sexual function is sensitive, the questionnaire was filled and sealed in an envelope.
The number of participants needed was calculated according to Cohen’s sampling formula using the sample size calculation program G*power 3.1.3. Based on the calculation results, with a correlation analysis significance level of 0.05, a medium effect size (d) of 0.30, and a power of 0.95, the minimum sample size required for this study was 64.
Measurement
Lower Urinary Tract Symptoms
To measure LUTS, we used a tool that verified the validity of Oh, et al. [12] in the Korean version of the Scored Form of the Bristol Female Lower Urinary Tract Symptoms Questionnaire developed by Brookes et al. [13]. The instrument consisted of a total of 12 items, consisting of four filling symptom items, three voiding symptom items, and five incontinence symptom items, with a minimum of 0 and a maximum of 47 items. The higher the score, the greater the degree of LUTS. The reliability Cronbach’s alpha coefficient at the time of development of this tool was .66 ~ .75. The Spearman-Brown coefficients in this study were filling symptom .71, voiding symptom .66, and incontinence symptom .52.Sexual Function
The FSFI (Female Sexual Function Index) developed by Rosen et al. [14] and translated into Korean [15] was used. The FSFI consists of a total of 19 questions in 6 domains: 2 questions related to sexual desire, 4 to sexual arousal, another 4 to vaginal lubrication, 3 to orgasm, 3 to satisfaction, and 3 to pain during intercourse. The domain-specific score is multiplied by the weighted value for each factor, and the scores for all 6 domains are added together to calculate the total sexual function score. The range of measured scores showed a distribution from a minimum of 2 to a maximum of 36. Higher scores signify that the perceived sexual function of the subject is higher. At the time of development, the Cronbach’s alpha coefficient was 0.97 in the research of Rosen et al. [14], in this study Cronbach’s alpha coefficient was .99.Quality of Life
In order to measure QoL, we used the Medical Outcomes Study 36- Item Short Form Version 2 Standard (SF-36v2) developed by Ware and Sherbourne [16] and validated by Quality Metric Incorporated in Korean. This tool had a total of 36 items with 5 items on general health, 10 on physical function, 4 on role-physical, 2 on bodily pain, 4 on vitality, 2 on social functioning, 3 on role-emotional, 5 on mental health, and 1 on overall health status. The physical QoL of 15 items and the mental QoL of 10 items are divided again. Score using Health Outcomes Scoring Software 5.0. From 0 to 100, the higher the score, the higher the QoL. The Cronbach’s alpha coefficient at the time of development of this tool was 61 ~ .89 [16]. In this study, physical QoL was .83, and mental QoL was .80.General Characteristics
The questionnaire form contained 13 questions concerning age, education, duration of marriage, number of vaginal deliveries, menopause, postmenopausal period, Kegel’s exercise, sexual intercourse, and types of UI.Data Analysis
The statistical software package SPSS/WIN 23.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. A 5% level of statistical significance was used. The general and clinical characteristics of the participants are expressed in real numbers and percentages. To express the participants’ degrees of LUTS, sexual function, and QoL, the real numbers and percentages, and means and standard deviations were computed. The differences in scores between LUTS, sexual function, and QoL according to the participants’ general and UI-related characteristics were analyzed using the independent t-test, one-way ANOVA, and post hoc Scheffe’s test and Dunnett T3 teat. Finally, the relationship between LUTS, sexual function, and QoL was analyzed using Pearson’s correlation coefficient.Results
General characteristics
Mean age of Women with UI was 53.34±11.11 years and 59.4% (n = 76) had attained at least high school-level education. Mean duration of marriage was 326.14±13.99 months and the highest number of subjects were found in the 241~420 months range (n=51, 39.8%). The average number of vaginal deliveries was 1.33±0.04 and 74 subjects (57.8%) had one or two vaginal deliveries. Menopause had set in for 83 subjects (64.8%), postmenopausal period would set in 80.20 ± 8.41 months, and for 67 subjects (52.3%), it would set in within 60 months. In Kegel’s exercise, 44 (34.4%) did not exercise. The average of sexual intercourse per month was 1.85 ± 0.07 times, and 1 or 2 times for 53 subjects (41.4%). About 55% of the participants were identified as women with UI. Stress UI was 54.7% and the proportion of urge UI and mixed UI was 13.3% and 32.0%, respectively.Mean Differences in LUTS, sexual function, and Physical and Mental QoL according to the General Characteristics
Among the LUTS scores according to the general characteristics, significant mean differences exited with respect to education level, menopause, postmenopausal period and types of UI. And among the sexual function scores according to the general characteristics, significant mean differences exited with respect to age, education level, duration of marriage, menopause, postmenopausal period, Kegel's exercise, sexual intercourse per months and Types of UI (Table 1).
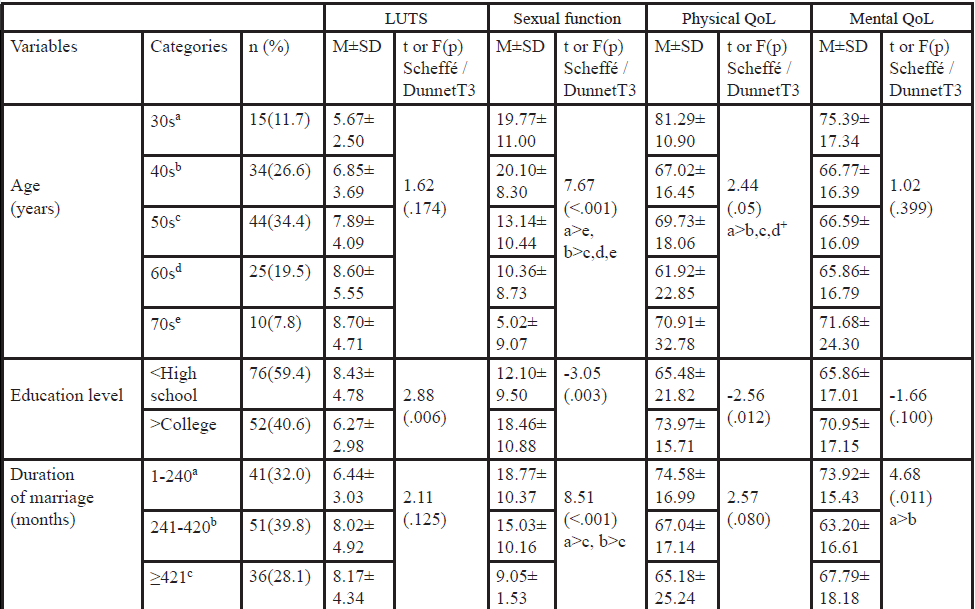 Table 1: Mean Differences in Physical and Mental QoL according to the General Characteristics (N=128).
Table 1: Mean Differences in Physical and Mental QoL according to the General Characteristics (N=128).+ Dunnet T3 test; LUTS=lower urinary tract symptoms, QoL=Quality of life, UI=Urinary incontinence
LUTS, Sexual Function, and QoL Scores
Total LUTS score was 7.55±4.27 (range 0–47) and the score for subfactors was 3.00±2.13 for filling symptom (range 0–15), 1.00±1.27 for voiding symptom (range 0–12), and 3.55±2.00 for incontinence symptom (range 0–20). The total score for the Sexual function was 14.67±10.52 (range 2–36) and scores for sub-factors were 2.21±1.05 for sexual desire (range 1.2–6), 2.06±1.85 for sexual arousal (range 0–6), 2.60±2.26 for lubrication (range 0–6), 2.31±2.04 for orgasm (range 0–6), 2.68±1.61 for sexual satisfaction (range 0.8–6), and 2.83±2.37 for sexual pain (range 0–6). The total score for physical and mental QoL were 72.21±18.51 (Range 0–100) and 77.78±15.98 (range 0–100), respectively (Table 2).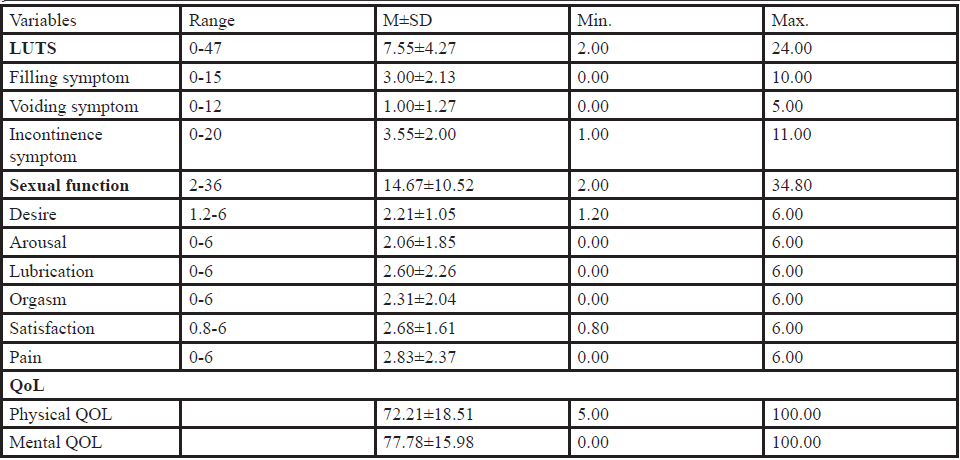 Table 2: LUTS, Sexual Function, and QoL Scores (N=128).
Table 2: LUTS, Sexual Function, and QoL Scores (N=128).LUTS=lower urinary tract symptoms, QoL=Quality of life, M=Mean, SD=Standard deviation
Correlation among the LUTS, Sexual Function, and QoL
LUTS has a statistically significant negative correlation with sexual function, physical QOL, and mental QoL, respectively, (r=-.234, p=.008); (r=-.486, p<.001); and (r=-.445, p<.001). Sexual function has a statistically significant positive correlation with physical and mental components of QoL, respectively, (r=.322, p<.001) and (r=.360, p<.001) (Table 3).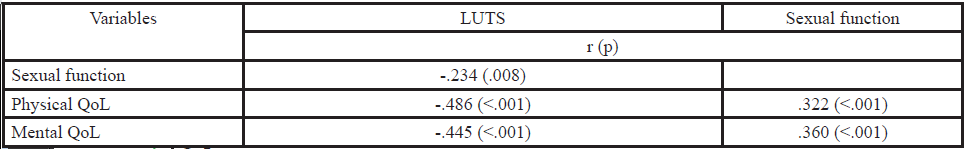 Table 3: Correlation among LUTS, Sexual Function and QoL (N=128).
Table 3: Correlation among LUTS, Sexual Function and QoL (N=128).LUTS=lower urinary tract symptoms, QoL=Quality of life
Discussion and Conclusion
The purpose of this study was to investigate the relationship between LUTS, sexual function and QoL and lower in married women with urinary incontinence.In this study, the prevalence according to the type of incontinence in married women was 54.7% for stress UI, 13.3% for urge UI, and 32.0% for mixed UI. The prevalence of UI in previous studies varied according to subject selection and data collection methods. The incidence of UI in this study was similar to that of a previous study [17]. The incidence of urinary incontinence was 55.7%, the incidence of stress UI was 60.8%, the urge and mixed UI were reported to be 1.0% and 38.2%, respectively [17]. However, according to the results of a population-based sampling study of adult women of the same age range (range 30 to 79 years) as in the present study, the incidence of UI was 41.2%, including stress UI (37.8%) and urge UI (14.9%) [12], and the prevalence of UI was lower in this study. The reason for the difference in the prevalence of urinary incontinence in this study is the age associated with incontinence incidence. In the Oh et al. [12] study, mean age was 51.1±12.8 years, while the mean age of women in this study was 53.34±11.11 years. For this reason, the prevalence of incontinence seems to be low. There was a difference in prevalence according to the type of UI, but it is consistent with the fact that stress UI is relatively higher than other types. However, the prevalence of UI in this study and previous studies is different because different tools have been used to determine UI. Thus, in future studies, it may be necessary to identify variables related to UI using objective indicators.
In this study, we discuss the level of LUTS, sexual function, and the QoL of married women who have UI. First, the LUTS score for women with urinary incontinence was 7.55±4.27 points out of 47 points. The results of this study showed that BFLUTS-SF, which uses the same tool as this study, showed LUTS score to be more than the result of 8.38±2.81 points, which is the LUTS score after menopausal transition [18]. Lower estradiol levels during menopausal transition lead to LUTS.
In previous studies, the ratio of menopausal and postmenopausal women was 95% and the rate of fertility was 3.2±2.1, which was related to the development of LUTS.
In this study, sexual function scores of married women with UI were 14.67±10.52 points out of 36 points. In a study of urologic patients using the same tool, 20.48±6.20 points [19], and a sexual function score of 22.39±2.09 points in patients with UI in Korea [20]. The sexual function scores in this study were significantly lower than those in previous studies [19,20]. As a result of comparing the general characteristics of the study subjects with the previous studies and sexual function scores, it was found that the average age of the sexual function, the number of menopausal women, and 47 cases (37.6%), respectively. Because of these differences in general characteristics, sexual function scores in this study seem to be significantly lower. In addition, the sexual function score of this study was 14.67 ± 10.52, which was significantly lower than the cutoff score of sexual dysfunction (26.6 points) [21] suggesting that there are many women with sexual dysfunction. In this study, many of the subjects with UI might be thought to have sexual dysfunction.
In the present study, the QoL scores for women with UI were 68.27±1.60 points out of 100 points. The results of this study were similar to those of previous studies in that the QoL of the women with UI was measured by SF-36, the tool that is also used in the present study, with a score of 69.0±10.6 [22].
In this study, the LUTS, sexual function, and QoL according to the demographic and UI - related characteristics of married women with UI was related to various sociodemographic and UI - related factors. In conclusion, this study should develop a nursing intervention program that can improve the three variables considering the demographic and UI-related characteristics reported to be associated with LUTS, sexual function, and QoL in married women with UI.
The results of this study showed that LUTS was correlated negatively with sexual function and QoL, and sexual function was positively correlated with QoL. That is, the more severe symptoms of lower urinary tract, the lower the sexual function and the QoL, and the better the sexual function, the higher the QoL. The results of this study suggest that there is a negative correlation between LUTS and the QoL of older women in the local community [23], and there is a positive correlation between the sexual function and the QoL of Turkish women with UI [24].
These results suggest that when sexual function and QoL in women with UI is severe are decreased. The LUTS, sexual function and quality of life of women with UI were found to be related to each other. Based on the results of this study, it is expected that nursing education and intervention programs should be introduced in nursing practice of the community to improve the identification of UI, sexual function, and the QoL of married women.
Acknowledgment
NoneConflict of interest
The authors declare no conflict of interest.Consent Statement
The author gives permission to Gexin publications for publication of this manuscript in the online Journal of Comprehensive Nursing Research and Care.References
- Haylen BT, de Ridder D, Freeman RM, Swift SE,
Berghmans B, et al. (2010) International urogynecological
association; international continence society. An international
urogynecological association (IUGA)/International Continence
Society (ICS) joint report on the terminology for female pelvic
floor dysfunction. Neurourol Urodyn 29: 4-20.View
- Nigam A, Ahmad A, Gaur D, Elahi AA, Batra S, et al. (2017)
Prevalence and risk factors for urinary incontinence in pregnant
women during late third trimester. Int J Reprod Contracept
Obstet Gynecol 5: 2187-2191.
View
-
Avery JC, Gill TK, Taylor AW, Stocks NP (2014) Urinary
incontinence: Severity, perceptions and population prevalence
in Australian women. Australian & New Zealand Contin J 20:
7-13.
- Abrams P, Blaivas JG, Stanton SL, Andersen JT (1988)
Standardization of terminology of lower urinary tract function.
Neurourol Urodyn 7: 403-427.View
- Shin CW, Kim SD, Cho WY (2009) The Prevalence and
Management of Urinary Incontinence in Elderly Patients at
Sanatorium in Busan Area. Korean J Urol 50: 450-456.
View
- Fultz NM, Burgio K, Diokno AC, Kinchen KS, Obenchain R, et
al. (2003) Burden of stress urinary incontinence for communitydwelling women. Am J Obstet Gynecol 189: 1275-1282.
- Kim SH, Kim HY (2018) Sexual Function and Quality of Life
in Urinary Incontinence and Non-urinary Incontinence Groups
of Married Women. Asia-pacific Journal of Multimedia Services
Convergent with Art, Humanities, and Sociology 8: 605-616.
- Chen G, Lin T, Hu S, Chen Y, Lin L, et al. (2003) Prevalence
and correlation of urinary incontinence and overactive bladder
in Taiwanese women. Neurourol Urodyn 22: 109-117.
- Kim JS, Lee EH (2003) Treatment-Seeking Behaviors and
Quality of Life among Community-Dwelling Older Women
with Urinary Incontinence. Hanguk Nonyonhak 23: 33-47.
- Kim M, Lee S (2008) Prevalence Rate and Associated Factors
of Urinary Incontinence among Nursing Home Residents. J
Korean Acad Nurs 38: 92-100.
View
- Kim OK, Yun H (2013) Prevalence of Urinary Incontinence,
Single Voided Volume, Post Void Residual Volume, Daytime
Frequency, and Nocturia in Women over 40 Years. Korean J
Adult Nurs 25: 679-689.View
- Oh S, Park WH, Park CH, Paick JS, Seo JT, et al. (2003)
Prevalence of Urinary Incontinence and Incontinence-related
Quality of Life in Korean Women: A Population-based Study.
Int Neurourol J 7: 73-80.View
- Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P, et al.
(2004) A scored form of the Bristol Female Lower Urinary Tract
Symptoms questionnaire: data from a randomized controlled
trial of surgery for women with stress incontinence. Am J Obstet
Gynecol 191: 73-82.View
- Rosen R, Brown C, Heiman J, Leiblum S, Meston C, et al. (2000)
The Female Sexual Function Index (FSFI): a multidimensional
self-report instrument for the assessment of female sexual
function. Sex Marital Ther 26: 191-208.View
- Kim HY, So HS, Park KS, Jeong SJ, Lee JY, et al. (2002)
Development of the Korean-version of Female Sexual Function
Index (FSFI). World J Mens Health 20: 50-56.View
- Ware Jr J, Sherbourne CD (1992) The MOS 36-item short-form
health survey (SF-36). I. Conceptual framework and item 80
selection. Medical Care 30: 473-483.View
- Song HJ, Lee DH, Lee JY, Kim MJ (2001) Epidemiologic Study
of Urinary Incontinence for Korean Women over 30 Years old.
Int Neurourol J 5: 24-38.
- Gopal M, Sammel MD, Arya LA, Freeman EW, Lin H, et al.
(2008) Association of Change in Estradiol to Lower Urinary
Tract Symptoms during the Menopausal Transition. Obstet
Gynecol 112: 1045-1056. View
- Sen I, Onaran M, Aksakal N, Acar C, Tan MO, et al. (2006) The
impact of urinary incontinence on female sexual function. Adv
Ther 23: 999-1008.
View
- Kim M (2013) Factors Influencing the Sexual Function of
Women with Urinary Incontinence. Korean J Women Health
Nurs 19: 108-118.
View
- Wigel H, Meston C, Rosen R (2005). The Female Sexual
Function Index (FSFI): Cross-validation and development of
clinical cutoff scores. Sex Marital Ther 31: 1-20.
View
- Kim HJ, Lee HS, Lee SH (2003) The Impact of Urinary
Incontinence on the Quality of Life in Women. Korean J Fam
Med 24: 709-714.
- Kweon Y, Kang Y (2012) Lower Urinary Tract Symptoms and
Incontinence Quality of Life among Middle Aged and Elderly
Women. Womens Health 13: 21-37.
- Ozkan S, Ogce F, Cakir D (2011) Quality of life and sexual
function of women with urinary incontinence. Jpn J Nurs Sci
8: 11-19.
View
Comments
Post a Comment